Promising advancements in CAR T-cell therapy for large B-cell lymphoma (LBCL) include potential new safety parameters, opportunities for precision care, and increased chances of achieving remission for some people.
LBCL is a type of non-Hodgkin’s lymphoma (NHL), a cancer that affects B cells in the lymphatic system. B cells are a type of lymphocyte that produce antibodies in response to pathogens, such as bacteria or viruses. When B lymphocytes grow and spread uncontrollably in LBCL, they can accumulate in organs and tissues, crowding out other healthy immune cells.
LBLCs are a fast-growing type of NHL, and diffuse LBLC (DLBLC) is the
Chemotherapy has traditionally been the frontline treatment for LBCL. Doctors use a combination of drugs known as the R-CHOP regimen to help stop cancer’s growth and spread. Radiation therapy and stem cell transplants are also a part of standard care.
When first-line treatments are ineffective, doctors consider alternative options. Chimeric antigen receptor (CAR) T-cell therapy is a
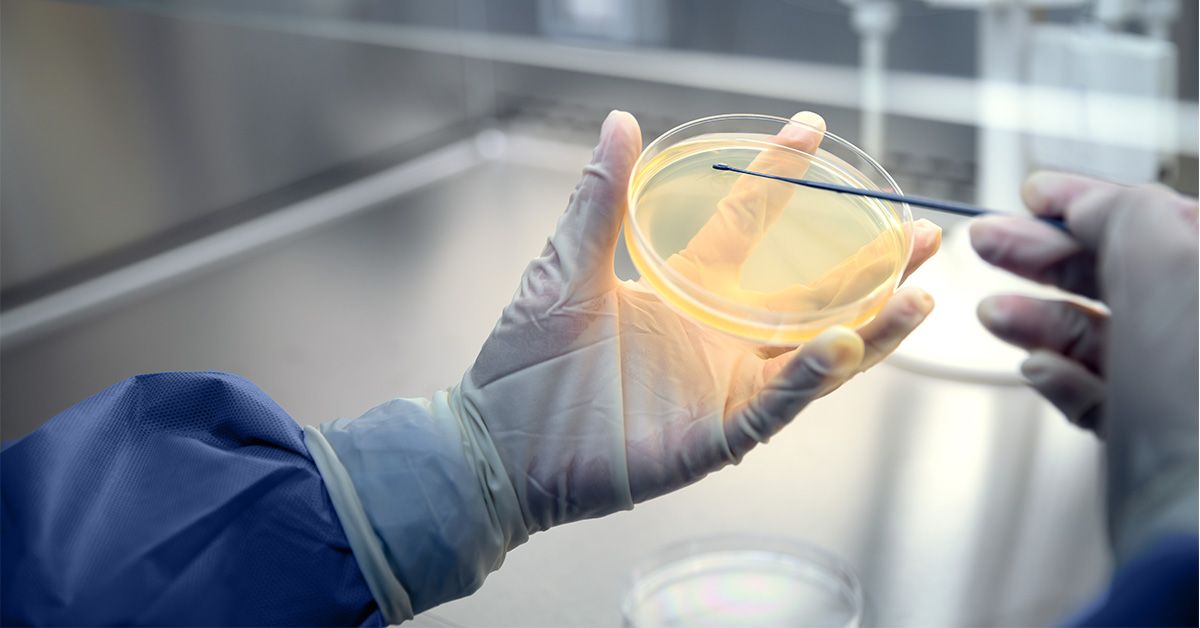
CAR T-cell therapy involves a healthcare professional collecting a person’s blood in a lab. The blood contains lymphocytes (including T lymphocytes), which are genetically modified to contain special receptors known as CAR. These receptors are capable of detecting and killing cancer cells.
This article examines some of the latest advancements in CAR T-cell therapy for LBCL.
In the largest
These microenvironments, which feature unique characteristics such as the presence of fibroblasts, support cells, or exhausted T cells, can help predict a person’s treatment response to specific therapies.
In the 2025 study, CAR T-cell therapy was found to be the most effective for people in the “lymph node” microenvironment group. These people already have abundant T cells present with plenty of other cells (support cells) that work to keep T cells healthy and active.
The findings provide new insights into lymphoma biology that could inform clinical approaches toward personalized, precision care in LBCL.
In a 2025
The findings help expand treatment eligibility and could provide older patients with a potentially curative option where one was not previously available.
Prior to this research, little data existed on CAR T-cell therapy in older adults, and newer treatment options weren’t always accessible due to complicating factors like co-existing medical conditions and age-related immune decline.
Traditional CAR T-cell therapy works by helping immune cells recognize a
CD19-only targeting therapy is effective, but it does not always catch all cancerous LBCL cells. Some cells may have CD19 mutations or may have lost their CD19 antigen. When this happens, cancer can relapse (return) because the CAR T-cells are no longer effective at recognizing it and removing it.
To help address this challenge, researchers developed dual-targeting CAR T-cell therapy, which allows T cells to recognize both CD19 and CD20 antigens on B cells.
In summer 2025, results from an ongoing Phase 1b clinical trial showed a high response rate for dual-targeting CAR T-cell therapy among people with relapsed or refractory (difficult to treat) LBCL.
The findings may help establish a broader range of efficacy for CAR T-cell therapy, reducing relapse rates and improving remission.
Cytokine release syndrome (CRS) and lymphodepletion are two of the most common complications of traditional CAR T-cell therapy that can limit its availability for certain people.
Lymphodepletion involves a short course of chemotherapy to eliminate healthy immune cells to make room for engineered T cells. It is a necessary part of conventional CAR T-cell therapy, but it temporarily lowers a person’s immunity, increasing the risk for infection.
CRS is a side effect that occurs when the sudden die-off of cancer cells from infused CAR T-cell therapy releases high levels of inflammatory substances, known as cytokines. CRS can cause fever, chills, and a headache, but it can also lead to potentially life threatening responses such as too-low blood pressure.
Both CRS and lymphodepletion arise from the ex vivo process of making traditional CAR T-cells, which means they are produced outside the body, in a laboratory.
In a 2025 case study, researchers demonstrated that in vivo CAR T-cell engineering may hold the key to eliminating the need for lymphodepletion and reducing the risk of CRS.
In vivo engineering uses gene therapy to modify T cells inside the body. This allows them to expand in a controlled manner, reducing their competition with existing immune cells. The slower expansion can also help prevent CRS by allowing cancer cell destruction to occur gradually, rather than suddenly at the time of an infusion.
The case study could pave the way for greater safety profiles in CAR T-cell therapy for LBCL.
In some people, LBCL spreads to tissues outside the lymph nodes, a condition known as extranodal (EN) disease.
According to a 2025 retrospective analysis, EN disease is associated with worse outcomes and lower treatment response to CAR-T cell therapy. Researchers explain that certain EN sites may naturally reduce the effectiveness of CAR-T cells and increase the likelihood of experiencing CRS.
Debulking EN disease by targeting specific organs with radiation before CAR T-cell therapy may improve outcomes.
These findings could offer doctors a new way to customize treatment plans based on a person’s unique LBCL diagnosis.
CAR T-cell therapy for LBCL modifies a person’s immune cells to help them identify and destroy cancerous B cells. Considered a second or third-line treatment option, doctors use CAR T-cell therapy when LBCL is not responding to traditional treatments or has recurred.
New advancements in CAR-T cell therapy include those that improve safety, efficacy, and precision care.
Share this article
OUR BRANDS